Abstract
Introduction
RAS mutations are subclonal events associated with both good and bad prognosis AML categories (Papaemmanuil E et al.N Engl J Med 2016; 374). An adverse prognostic meaning of RAS mutations in treated AML with myelodysplastic-related changes has also been reported.In solid tumors, it has been shown that patients with KRASQ61K do not confer resistance to therapy, unlike other mutations: KRASQ61K introduces a cryptic splice donor site and causes a short inactive isoform (Kobayashi Y et al. Nature 2022 ;603). However, most KRASQ61K patients acquired the silent mutation G60G, which removes the new splice donor site and increases therapy resistance. This splicing mechanism was not present in cases with NRASQ61K and HRASQ61K. We investigated the frequency of RAS mutations, their molecular associations, and the prevalence of splicing mechanisms involving KRASQ61K and NRASQ61K in AML.
Methods
We included a consecutive series of adult de novo AML enrolled in the CETLAM trials, a total of 620 patients who were diagnosed between 2017 to 2022. DNA and RNA were extracted from bone marrow or peripheral blood. Next Generation Sequencing (NGS) was carried out with three panels containing at least 42 AML-related genes, including KRAS and NRAS. Only variants with a VAF (variant allele frequency) >4% and ranked as pathogenic or likely pathogenic were used for the analysis. Conventional karyotype was routinely assessed. cDNA was obtained from 7 patients with NRASQ61K, and was amplified through a conventional PCR. cDNA products were observed in gel electrophoresis and sequenced by the Sanger method. IBM SPSS Statistics was used to perform Chi-Square tests. In statistical tests regarding molecular associations, patients with co-mutated NRAS and KRAS are excluded.
Results
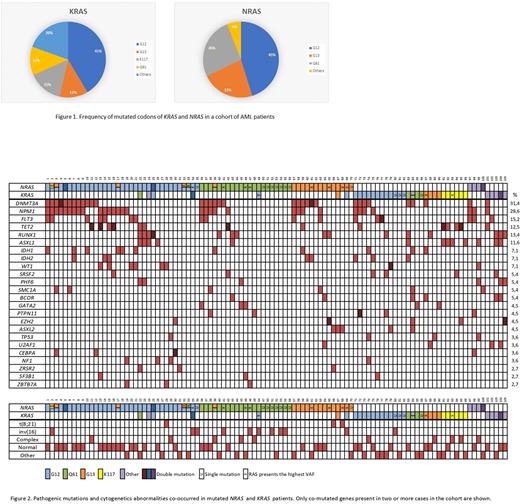
Our study found RAS mutations in 16.9% (105 patients) of adult AML cases. 11.9% of AML patients had mutated NRAS, while 6.1% mutated KRAS (74 and 38 patients, respectively). In our study, Q61 was the third most common mutation in NRAS with an incidence of 26%, while it was the fourth most common in KRAS with a frequency of 12%. The distribution of mutations in KRAS and NRAS is shown in figure 1. Regarding the Q61 codon, the distribution of each amino acid change in our cohort is shown in Figure 1b. Nine NRASQ61K were found, and cDNA could be obtained from 7 patients. NRASQ61K and non-mutated NRAS samples presented the standard large transcript in the gel electrophoresis. These findings ruled out the presence of exon skipping in AML with NRASQ61K mutations. No single case of KRASQ61K was observed in this extensive series of AML, so we could not identify alternative transcripts described in solid tumors nor compensatory KRASG60G mutations.1.1% of patients (7 cases) presented co-mutated NRAS and KRAS. In 9 subjects, more than one NRAS mutation was found, whereas, in 3 patients we detected two KRAS mutations. Lastly, we focused on molecular associations of RAS mutated patients (Figure 2). Of the total RAS-mutated cohort (105 patients), DNMT3A and NPM1 had the highest mutation frequency. Notably, 40.3% of NRAS-mutated patients had NPM1 mutations, significantly higher (p=0.018) than KRAS (16.1%). Another interesting finding was that KRASK117N mutations were mutually exclusive with DNMT3A and NPM1. All KRASK117N (6 cases) were associated with TET2 and or ASXL1 mutations. Cytogenetics information was available for 87 patients with RAS mutations (59 NRAS and 35 KRAS). NRAS-mutated patients showed a higher frequency of core binding factor (CBF) alterations than KRAS (18.1% vs. 3.6%, respectively) (p=0.063). Complex and miscellaneous karyotypes had higher rates of KRAS mutations than NRAS mutations (57.1% vs. 32.7%, respectively, p=0.032).In 26 cases, RAS mutations were the single mutation or the one with the highest VAF; notably, 42.3% had an NRASQ61 mutation. We had cytogenetic information of 20 patients, and twelve had inv(16) (60%).
Conclusions
In this cohort of adult AML cases, RAS mutations were present in 16.9%. Mutations at codon G12 were the most prevalent lesions in AML. NRAS mutations were more frequent than those of KRAS. Up to 17% of RAS mutated AML cases showed more than one mutation. CBF chromosomal abnormalities were commonly associated with NRAS mutations. Complex and miscellaneous karyotypes showed KRAS mutations more often. KRASK117N mutations were consistently associated with TET2 and ASXL1 mutations and mutually exclusive with NPM1 and DNMT3A.
Disclosures
Castellet:Pfizer: Current Employment. Pratcorona:Novartis: Honoraria. Arnan:MNS, JAZZ, Novartis, Abbvie: Consultancy, Speakers Bureau. Sampol:GSK: Consultancy. Salamero:Abbie, BMS, Novartis: Consultancy, Honoraria. Esteve:Pfizer: Research Funding; Novartis: Honoraria; Jazz: Research Funding. Sierra:Pfizer: Research Funding; Novartis: Honoraria; Jazz: Research Funding. Nomdedeu:Novartis: Honoraria; Abbvie: Honoraria; Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.